
Walter’s way forward
Walter Massett was an early walker, taking his first steps at 10 months old. By March 2020, just shy of his second birthday, Walter’s mom, Rae-Anne, noticed Walter having some trouble with his balance and mobility.
“When I would finish changing his diaper, I’d set him down and I’d notice him teetering a little,” Rae-Anne, who lives in Kingston, Ont., recalls.
Walter had frequent ear infections, so Rae-Anne thought it could be yet another one throwing off his balance. He’d also been crying more than usual, with occasional vomiting, and wanting to be carried, all things that could be explained away by an ear infection or simply Walter’s stage of life.
“He had a long history of vomiting, sometimes for known reasons but sometimes not,” Rae-Anne says. “As he was still so young and somewhat delayed in language, we assumed crying was just part of being a toddler. It could typically be soothed or redirected. We also figured that wanting to be carried everywhere might have just been him being tricky with us—part of the ‘terrible twos’ era we were in.”
The first doctor visit
 Walter had been on the wait list to see an ear, nose and throat (ENT) specialist, but Rae-Anne called the doctor to see about getting him a prescription for antibiotics in the meantime.
Walter had been on the wait list to see an ear, nose and throat (ENT) specialist, but Rae-Anne called the doctor to see about getting him a prescription for antibiotics in the meantime.
As it was the beginning of the COVID-19 pandemic, phone appointments were the norm. She spoke with a resident, who consulted with a doctor on staff.
“They came back and said, ‘Just because he’s so young and infections can cause a lot of issues, we think it’s a good idea for you to bring him in for a physical exam,’” Rae-Anne says.
She describes the doctor’s visit as overwhelming and intimidating, during a time when medical staff were dressed head-to-toe in protective garb, from gowns to masks, gloves and face shields. Walter’s exam revealed some redness in his ear, and so the doctor agreed to antibiotics.
“I was ready to go home,” Rae-Anne says. “We were walking down the hall and apparently Walter’s gait got the doctor’s attention. He was actually willing to walk that day, which was incredible.”
“To me, the way he walked was normal, like any little kid would walk. But, I didn’t see things the same way the doctor did.”
Trying to find the cause
The doctor asked Rae-Anne and Walter to return to the exam room, where he advised that Walter be seen at the Children’s Outpatient Clinic (COPC).
“I went from being kind of relaxed and chill, thinking this is just an ear infection, to thinking, ‘Something’s really wrong,’” Rae-Anne says.
Rae-Anne took Walter to the COPC where he saw a doctor, who Rae-Anne later learned was a pediatric oncologist. Walter went through several tests before being kept overnight at Kingston General Hospital for observation.
“They had so many questions like, ‘Has he ingested any chemicals? Do you have lead paint?’” Rae-Anne says. “It was really stressful because I kept thinking, ‘Have I done something wrong?’”
Rae-Anne mentioned the frequent vomiting, though noted that Walter had always vomited a lot, as is common in babies with reflux. He’d also had frequent colds, which again, isn’t unheard of in kids who share toys—and germs—in daycare.
The doctor told Rae-Anne it was likely acute cerebellar ataxia, which is a sudden loss of muscle co-ordination that’s often caused by a viral infection. She was told to follow through with the antibiotics, which seemed to help for a brief time.
“Then, as quickly as we saw that improvement, he regressed,” Rae-Anne says. “Crawling was preferred over walking, and being carried was preferred over crawling.”
A mother’s fight
 It was back to the doctor for Walter, who again, went through several tests to determine what could be going on.
It was back to the doctor for Walter, who again, went through several tests to determine what could be going on.
“I was told, ‘Well, we can’t see anything wrong, so we’ll have to put in a referral for a pediatric neurologist,’” Rae-Anne says. “I had such strong feelings, I can’t even describe it, but I said, ‘No, I’ve been waiting over a year for the ENT referral and I’m not willing to wait for a neurology referral.’”
“I’d been questioning things for a while, but by then it was clear to me that something was really wrong.”
Rae-Anne took Walter back to COPC, where he was again, tested and examined, and ultimately, sent to Kingston General Hospital for another overnight stay, so he could have an MRI first thing in the morning.
“It broke my heart because my baby, he couldn’t eat or drink, and I’m so used to making sure he has all those needs met,” Rae-Anne says. “He wanted to eat and drink, but I had to keep refusing, and it wasn’t until noon the next day that they finally did the MRI.”
Walter’s head circumference was also a concern, with Rae-Anne noting Walter’s growth had always been “off the charts.”
“His head circumference, in particular, became a focus once readmitted and waiting for his first MRI at Kingston General Hospital,” she says. “It was found to be above the 99th percentile at that point.”
“These days,” she adds, “his big head means he fits hats and toques that belong to me and his dad—something we often laugh about.”
At that point, however, Walter’s condition was far from a laughing matter, as his family awaited his MRI results.
Walter’s MRI
Rae-Anne met Walter in his hospital room after the MRI, and was thrilled to see the nurse had brought him apple juice and a cheese sandwich. That’s when the pediatric oncologist she’d initially spoken to joined them and asked to have a word with Rae-Anne and her partner, Brad, in another room.
“I had this flooding panic because they don’t usually ask for you to go somewhere to talk,” Rae-Anne says. “We went down the hall to this nice room, with couches, big windows and a waterfront view. That’s when the doctor said, ‘We see a brain tumour.’”
Stepping into the whirlwind
 Walter’s tumour measured more than 7.5 cm—larger than a baseball. It had caused a buildup of fluid and was pushing his brain to the left, dangerously close to his brainstem.
Walter’s tumour measured more than 7.5 cm—larger than a baseball. It had caused a buildup of fluid and was pushing his brain to the left, dangerously close to his brainstem.
“Hearing that our toddler had a brain tumour was one of the most disorienting and terrifying moments of our lives,” Rae-Anne recalls.
“It felt like the world blurred and the ground dropped out beneath us.”
Rae-Anne was told that Walter would need to go to SickKids in Toronto for surgery. What she didn’t expect was how quickly it was to happen, as Ornge, Ontario’s air ambulance service, was to pick Walter up in a matter of hours.
“I hadn’t noticed the helipad outside,” Rae-Anne says, “but I became pretty aware of it shortly after we learned what Ornge was, and that they would be coming and landing there.”
Only one parent could join Walter, so it was decided that Rae-Anne would go, while Brad would pack up their belongings and find boarding for their dogs.
Brad arrived in Toronto around 11 p.m. that night, when Rae-Anne was meeting with the pediatric neurosurgeon and Walter was in pre-operation isolation.
“The surgeon said, ‘He’s going to be on the operating table at 8 a.m. tomorrow,’ and I’m like, ‘You’d better make sure you get enough sleep, that’s nine hours from now!’” she says.
Walter was to have a craniotomy, tumour excision, and external ventricular drain (EVD) inserted. The entire process would take six to eight hours, Rae-Anne was told.
“It was grounds for nail biting as we got into the ninth hour,” she says. “Then, the phone finally rang. All went just fine and he was in post-op recovery.”
“There are no words to describe how fortunate we are because, even though it was terrifying and there were so many unknowns, it went the best it possibly could,” Rae-Anne continues.
Walter’s recovery
Rae-Anne and Brad had to switch places while Walter was recovering in the ICU, due to the one-parent-at-a-time rule. Brad was there when Walter woke up, and recalls Walter saying, “No, no, no.”
“I can imagine he was really confused,” Rae-Anne says, of Walter. “He looked so vulnerable, bandaged up. And I got a picture of him smiling, but it was a very fleeting moment. A few days later, he said ‘Mama,’ and I hadn’t heard that in a week, so that was exciting.”
For a few days after surgery, Walter would have tremors when he drifted off to sleep, which would startle him awake.
 “I don’t think he slept more than five minutes without this happening,” Rae-Anne says. “The doctor would say not to worry about it and kept reminding me that I needed to rest myself, but it was so hard not to worry about Walter and continue to go down Internet rabbit holes, trying to absorb information to prepare for any possibility that may come our way.”
“I don’t think he slept more than five minutes without this happening,” Rae-Anne says. “The doctor would say not to worry about it and kept reminding me that I needed to rest myself, but it was so hard not to worry about Walter and continue to go down Internet rabbit holes, trying to absorb information to prepare for any possibility that may come our way.”
The family celebrated Easter in the hospital, with Rae-Anne scattering Easter eggs on Walter’s hospital bed because he hadn’t yet been able to spend much time sitting up. His medical team was still carefully testing how his body handled changes in pressure from cerebrospinal fluid (CSF), and he could only manage short periods upright.
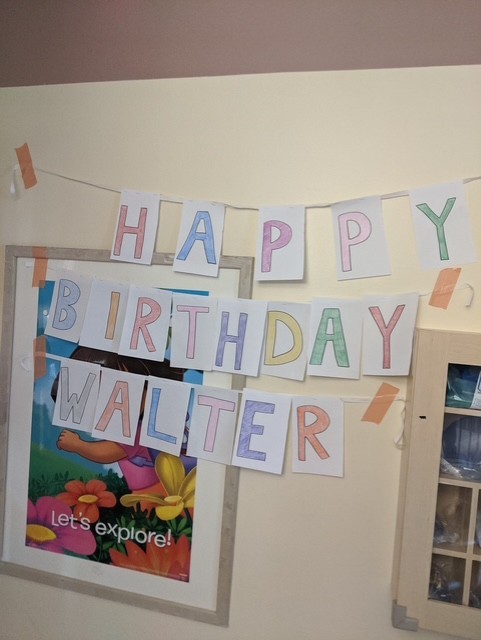
Two days later, on April 14, was Walter’s second birthday.
“The hospital staff made his day as special as they could, with decorations, a giant card, and presents,” says Rae-Anne. “Even I got a gift—the news that his EVD could come out and he didn’t require a second surgery for a shunt!”
On April 16, Walter was transferred to Holland Bloorview Kids Rehabilitation Hospital, where Rae-Anne learned that his tumour was a pilocytic astrocytoma, which was non-malignant and had a low likelihood of recurrence.
“While at SickKids, I asked several times about the result of the biopsy to learn the type of tumour, always hoping for a non-malignant finding,” Rae-Anne says. “I kept being told to wait, but was reminded that the resection was a perfect success and that I shouldn’t worry. It was a relief to find out for certain, once at Holland Bloorview, that this was the case.”
Walter stayed in hospital until May 28, working through occupational therapy and physiotherapy six days a week, along with speech therapy three days a week. After returning home, Walter was assessed by KidsInclusive acquired brain injury team. A continuance of speech therapy was the focus, which concluded in fall 2023.
The neurosurgery team at SickKids has been thorough with follow-ups, notes Rae-Anne. Walter had his first follow-up MRI at six months post-surgery, and then a year post surgery, and now every two years.
“We attended our last MRI in May 2024, and we now wait two years until the next,” Rae-Anne says. “Once we get to 2030—a decade post-tumour—we will celebrate in a big way, because that will be considered the goal post to be officially all clear!”
Tackling tumours with community
 Now seven years old, Walter is thriving.
Now seven years old, Walter is thriving.
“He’s funny, bright, and incredibly thoughtful,” says Rae-Anne. “He’s a deep feeler with a strong sense of fairness and justice. He’s a voracious reader, loves math, and is endlessly curious, especially when something captures his attention and he can dive deep into the details. He’s also a perfectionist who sometimes struggles when things don’t go to plan, but that passion is part of what makes him who he is.”
Walter doesn’t remember much from the early days of his journey, but he is starting to understand the impact of it.
“He talks about his scars, from his craniotomy and the external ventricular drain, with pride, often showing them off to others with a kind of quiet confidence,” Rae-Anne says. “He’s beginning to understand what it means to be a survivor, and we see that pride growing in him. It’s rare and remarkable.”
Walter has participated in Brain Tumour Walks with Rae-Anne since 2023, also taking part in this year’s Brain Tumour Walk in Kingston. He walked with the Kingston Grenadiers Football Club, which also made him an honourary captain for its annual Grens Tackle Tumours event.
Walter suited up with the team and scored the first touchdown of the game, helping to raise awareness and funds for those affected by brain tumours.
“We’re so lucky for Walter to have been saved and allowed to thrive, thanks to neurosurgeon Dr. Michael Taylor, amazing health-care providers, and top-notch therapists,” says Rae-Anne. “We want to share his story to offer hope, and remind others that even in the darkest moments, something beautiful and full of life might still be ahead.”