
Living with GBM – Sebastien’s Story
When I started getting headaches occasionally in May 2019, I assumed I must be getting dehydrated from my weekly intramural games.
I rarely used Advil or Tylenol for headaches unless dealing with a serious hangover, so I upped the water and started taking an electrolyte supplement.
The headaches became more regular and I started taking Tylenol or Advil, (I didn’t know the difference). The headaches would subside for a bit but started to occur more often. They weren’t bad and it was only a minor annoyance at the time.
Then one day in July I woke up to a throbbing headache and knew I wouldn’t be able to go to the office. Emily insisted that we go to the emergency room since I was having them so often. I thought the idea was ridiculous. My understanding of ER’s at the time was that it was a place for gunshot wounds and heart attacks.
But once at the ER, the throbbing got worse. They put me in a room with other visitors to wait for an assessment. I tried using others in the room as a distraction, one lady was gleefully telling everyone how she had broken her first bone but the pain in my head was making me nauseous. I went for a pee and threw up.
Our wait time decreased significantly after that.
The doctor saw us and asked me to describe my headaches and if had banged my head recently. He did basic tests to see for possible aneurysm symptoms.
He didn’t seem overly concerned so we weren’t either.
We got a CT scan which I thought excessive but also super cool. We waited and the doctor came back and asked to see me and Emily. I initially volunteered to see him alone but he said it was best she come with. First moment of hesitation.
He led us to his office, sat us down, and let us know the CT scan had revealed a mass about the size of a golf ball in my head.
Everyone has imagined winning the lottery before, and to that effect, most people have imagined being told terrible medical news. I definitely had. Some scenario where a doctor told me I had six months to live or something. When it actually happened it was surreal.
The kindness of the doctor, the shock, the tears. The experience was so similar to how I had imagined it, it felt like Déjà vu. The doctor went on saying “I am so sorry…” telling us that this was serious and that he would do everything he could.
We were crying but I wasn’t comprehending.
I felt like I was in a movie and that I would go back home and my life would carry on. The doctor told us he wasn’t sure what kind of tumour it was or if it was cancer or not. I would have to be transferred to another hospital, but he gave us a referral saying if I ever came back to that specific hospital, he would see me right away.
Obviously in shock, I remember being a bit pleased about his referral because that ER wait is a B and I wouldn’t want to sit through it again any time soon. I was put on a steroid drip, hooked up to a bunch of things and like that, it had started getting way too real. After notifying my family where I was going, I was transferred to the Ottawa Civic Hospital, which luckily has one of the best neurology departments in Canada.

Emily and I spent the night in the ER ward which was obviously not a restful night. Eventually a team of remarkably young physicians came to perform some cognitive tests on me and showed me the tumour in my head on a scan with no real conclusion of what it was or plan moving forward.
They were shocked that I was completely okay with a tumour that size in my head, that I had no obvious neurological deficiencies. I really didn’t – other than feeling like “WTF IS GOING ON! IT WAS ALL GOOD JUST A WEEK AGO,” I was fine. They told me I would be meeting with more doctors the next day and left, so I did what every normal person would do, and googled all I could about brain tumours. They tell you not to google, but you do.
None of the information helped and I was probably more confused afterwards.
I met with doctors over the next couple of days with intermittent visits from my family and friends. The bottom line was – I needed a plan. They decided that I would have surgery. Brain surgery. I honestly didn’t even realize how serious that was at the time. I didn’t even really know anyone who had surgery before.
The first neurosurgeon I met was kinda ‘meh’ about the whole thing and did not instill a lot of confidence in me or my family. I don’t know what happened or why he decided to hand over my case but we ended up meeting another surgeon and he was an absolute rock star.
He was a funny guy, but you could tell he was a professional and had a stellar record. He reassured Emily and my parents that he and his team would remove the tumour ASAP. I was scheduled in for surgery the following week. In hindsight, after having the chance to talk to someone who went through the same ordeal, it was good that it all happened so quick.
I barely even cared about the surgery leading up to it. I was much more concerned with the tumour in my head – I wanted it out.
They explained to me that the brain is very malleable and can create space in the cranium if a tumour is growing slowly, which mine had apparently. The headaches signaled that my skull was getting to the point that it could not accommodate any more tumour growth. My doctor was quite confident he would get a majority, if not all of it out.
The twist for the surgery is that I would be awake. Wait… what?
So, I would be conscious during brain surgery and actually “helping” them out during it – waking up at certain times to answer questions. Cool cool cool coooool. I spent the next days hanging out with Emily/friends/family.
The night before surgery I hung out with my uncle and cousins in the cafeteria, eating pizza. I slept relatively well but had some stomach issues and prayed that I would not need to poop during surgery (pizza had been a mistake). Morning came, I said bye to Emily and my family and was carted away. I met the team once again and they prepped me to go under.
They explained which drugs they would be using, when, and why, and how I would feel. I recognized fentanyl and ketamine but the rest were just words with a lot x’s and z’s. The anesthesiologist was impressed with how calm I was but if I had known what I was getting myself into it would have been quite different situation. Surgery was crazy.
At first it is run like a military exercise, everyone presenting themselves, listing off their roles and duties. Then the surgeon (Dr. Sinclair) gives an overview and timeline of the surgery. Very cool. Then I was out.
I woke up in the operating room feeling super chilled out.
They are about to do the drilling through my skull and asking me how I feel. I’m good. Real good. I don’t exactly recall what happened, but I felt the drilling. It wasn’t pleasant but it didn’t hurt. Then what I thought was the ketamine hits. I am tripping, HARD. I am at a bar with Emily that I know it is fake but it feels very real.
I can order drinks and talk to her but I also know I am having brain surgery. It was very weird and it got crazier but I don’t recall much of it. When I am woken up, Dr. Sinclair explains to me that he will be mapping my brain by poking the areas around my tumour with a wand-like object that sends electricity through my brain in order to see what he can and can’t remove.
Every time he does it on a part that is not tumour, I felt my hands or feet move. Apparently the part of the brain that was being operated on was responsible for my left side motor controls.
Once mapped, he removes the tumour with a mini vacuum that looks like a skinny pen, explaining everything to a Harvard student who had come for what I guess is the wildest work co-op ever.
The detail and confidence in his explanations showcased how intimately he knows the brain and his familiarity with the operation.
He starts talking to me, chatting me up about my interests and I’m probably giving him a terrible explanation of my travelling experiences over the last couple of years. He then asks what I would like to listen to. I request Justin Bieber, anything from the Believe era. Later on, we found a Justin we could agree on, Justin Timberlake.
“Can’t stop the feeling” becomes the main jam of the surgery. The craziness of jamming out to JT while having my brain operated wasn’t lost on me. After 9 hours, the doctor had removed 95 per cent of the tumour so that it wasn’t even visible on scans. I was brought to the ICU afterwards where I was dazed and struggled to breathe properly.
I was thirsty, irate, and couldn’t get enough air. I was given a bit of water and threw it up all over a nurse. I felt so guilty as they mopped me up. Heads up, nurses are the best. I know we’re hyper aware now with Covid, but it can’t be overstated.
It turns out, the time following the surgery was the hardest part. I moved back to the neuro ward and the following week I was in the worst pain I had ever experienced. The brain itself has no nerves for pain but the skull sure does. My head ballooned up from being drilled into and my head was four or five colours of bruising.
My brain was also hypersensitive.
I could not look at screens, the beeping of any of the hospital machines was agony, and even thinking too hard was a source of grief. The headaches were 10/10 pain. I was taking any drug they gave me to dull it. I would be in and out of sleep and the nights I would be wide awake until they dosed me with something that must be morphine or similar to it.
I realized in that state, how much processing our brain really does without us noticing. I did my best to think of nothing. (FYI The show Lennox Hill on Netflix goes into great detail about this surgery and has my almost exact surgery in episode 4 or 5 I think)
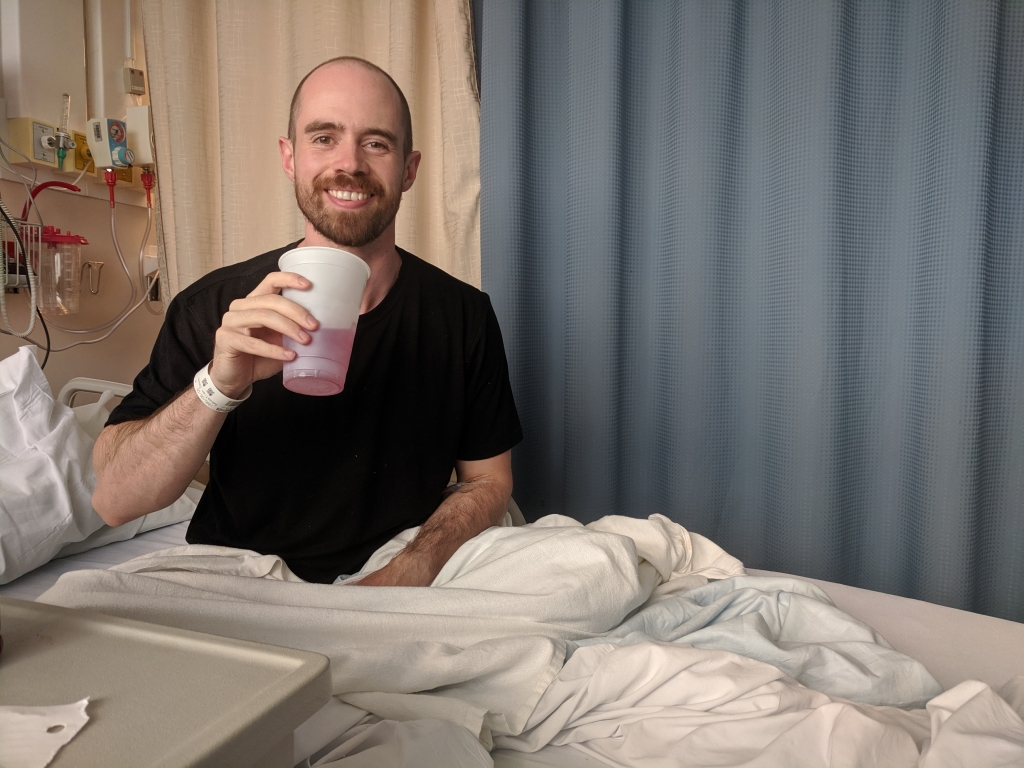
I spent two weeks recovering in the hospital. During my stay, my family was around bringing me food and just being present. Emily would come to cuddle and bring more food (I was on steroids to deal with the swelling and I was ravenous). You feel exceptionally lonely in these times and just having familiar faces around is joyous. I was also blessed with amazing nurses that were funny, diligent, and professional.
Overall, it takes 6-8 weeks to initially recover from brain surgery and countless follow ups. I had staples across my head, a big scar, and a deformed skull due to swelling (it’s back to normal now). I leaked blood from my head which led to a couple of pillows being thrown out. I was also just out of it.
Everything felt like a monumental task.
Due to the tumour placement, I was a bit unsteady on my feet and had to do some physio. Going from playing basketball weekly to learning how to use stairs again in the same month is demoralizing. I forced myself to practice walking whenever I could.
I stayed in the ICU ward for an additional week due to some swelling complications. The doctors doing rounds were mostly the same young ones I had met previously. It was hard not to be envious of their health. Did they know that I was just like them last month? Walking and talking without having to take a breather. Going for beers after work or to the movies for date night. To feel normal, I tried to pull off some banter with them whenever possible, and I felt the separation between doctor and patient ease a bit.
I was released from the hospital in August. My surgery took place July 23, though I’d been in the hospital since early July. They told me to keep it chill and to slowly work back into life. I stayed at my parents’ place in the country, where after weeks of hospital wards, I was mesmerized by nature – the wind, the fresh air, the space.
I tried to enjoy the last of the heat from summer but it was hard not to just sleep all day. When I did have energy, I pushed it too much. I am not patient with improvement. I pushed it too far one day, walked for a whole 15 minutes, and absolutely exhausted myself. When I made it back to the house I slept for the rest of the day and night.
It was going to be a slow go.
I went back to my place after a couple of days. I mostly slept and attempted little walks. The first time I walked to McDonald’s at the end of the street, sat down and ate my BLT bagel, it felt like a significant accomplishment. I was doing it, participating in society again.
However, I was far from back to normal. Soon after getting home, Emily and I went on our first date since the hospital at a local Italian place. I felt lost, bothered by flurries of activity, and had a horrible habit of stumbling. I had to relearn spatial coordination because I no longer really understood how big I was. I would bump into doorways and hit my head while getting in cars.
In addition, I had numbness in my hands and legs that I wasn’t sure would go away. It was all confusing/concerning/embarrassing for me.
No one had really explained to me the challenges I might face. It was a time of frustration and irritation, and it took me months to realize that what I had gone through wasn’t normal and that I would have to be patient with myself.
It was isolating because I had missed the entire summer and wanted to get back to my life. But even when I could hang out, I’d only be able to stand socializing for twenty minutes before I would be tuckered from the stimulation. I really valued friends who were cool about keeping things short and sweet.
I had been told that it was routine to meet a radiologist and oncologist after this surgery. Samples had been sent for analysis so we were waiting on those results to see if it was cancer or benign. I hoped it would be benign but unfortunately, that wasn’t the case.
We met the radiologist and he came out point blank and said the initial pathology indicated a glioblastoma. My heart dropped. He kept talking but I wasn’t listening.
This was far worse than even hearing about the tumour initially.
I knew about glioblastomas. I had googled them intensely and knew it was worst case scenario. My dad, who was just shocked about the cancer diagnosis, seemed to take it in stride, but I could feel the despair hitting me. I asked for the prognosis immediately, already knowing it wasn’t good, so that my dad had some sort of reference.
The doctor confirmed that five per cent of glioblastoma patients made it to five years, the median making it a year. My dad is the most chill, patient, emotionally stable person I know. Not that day. Vexed with the information he had just heard, he asked the doctor if he was telling his son that he would be lucky to live another year.
The pain/concern in his voice was probably harder to hear than the actual diagnosis. The doctor confirmed and I just felt lost. The shock was starting to set in. I had just turned 29 years old. I was in the midst of an amazing relationship, I had great friends with awesome summer plans ahead, and a good job with people I really enjoyed working with.
The doctor let me know I was going to be doing radiation for the next six weeks coupled with chemotherapy. He didn’t know that I had not been told yet, and it was an uncomfortable visit from that point on.
We met an oncologist who was somehow even less compassionate and gave us a more detailed prognosis with some pamphlets about clinical trials – as if I was of sound mind to leaf through and choose which immunotherapy trial might be best for me.
My dad and I left and sat in his truck, stunned.
Then we cried. After a long time, I called Emily and told her. I could barely explain it through my sobs and then hers. Then my dad and I made the trip home to do what we both knew would be the most difficult part in this.
My mom came home from the grocery store and I had to tell her that her only son who she had worked so hard to care for – who had finally started making his way – would be lucky to make it far into the decade, or even the next year. It was rough.
The pain of telling the ones closest to you is harder than hearing and facing the news yourself. It feels like you’re letting them down and directly causing them this pain. It takes time to realize that this isn’t your fault, and even though it sounds ridiculous you feel guilty for having cancer.

I felt guilty my mom might not have grandchildren, that all my parents’ hard work would be wasted if I died before them. The countless hours instilling lessons that eventually forged correctly, the hours worked to afford me special camps, clothes, trips. Even worse, they would have no one to help them when they were older.
It made me feel ashamed and lost.
However, my mom and dad were two of the strongest support systems I had during this time. They were there when needed and always made sure that I was doing my best in the given situation.
We met with my neurosurgeon the next day and he was a bit heated. He quickly explained that no one should have given me a prognosis and that the final pathology wasn’t even back yet (although it was a confirmed GBM). Doctors are great, but they aren’t always perfect. When you have three doctors assigned to you, there can be miscommunications. But my surgeon was perfect when it mattered.
At some point I will be a GBM statistic and it was hard to accept that in the beginning. You think that your life is uniquely important and that sure, people die from cancer everyday, but that won’t be me.
I’m too young. The odds are too great. A thousand people out of Canada’s 36 million people will be diagnosed with GBM this year. Furthermore, most of them will be over the age of 65 – too young still but a far cry from 29. I still had another lifetime to live.
I struggled with this a bit.
I was confused, and asked my doctor how I could have gotten this? Unsatisfying as it was, he explained this cancer was a genetic hiccup. Something just went wrong.
This was agonizing for awhile until you realize that the answer to the question “why me?” is only answered fittingly with the question “Why not me?”
Although rare, people win the lottery. It was difficult to accept that I had won the extremely rare brain cancer lottery. That was until I was at the hospital and a girl that looked 12 went in for the same brain cancer radiation I would be doing. The perspective change happened fast. If she can get this, then I can get this. So can anyone.
In fall 2019, I would get driven to the Civic hospital five days a week to have my head beamed with radiation with hopes of discouraging the cancer cells from multiplying. I am forever grateful to Emily’s family and mine who drove me each time. My support system was tiptop.
Radiation was weird but overall, I handled it well for the most part. Chemotherapy was a bit different. I had to do an oral dose, which is just a pill – but they look like mini nuclear matter pills.
They tell you to handle the pills very carefully and no one should touch them other than me, especially pregnant women. I had to quickly wash my hands thoroughly after touching the pills. Great, now that I know how toxic they are, lets pop these suckers into my body for the next six months.
The oral chemotherapy although not pleasant (or possibly even effective) could have been a lot worse. The first dose made things real. Chemotherapy is something I have associated with cancer for my whole life.
It was now official, I was a cancer patient.
The first dose was emotional, but it became routine over fall/winter. The treatment period was a tough time because I wasn’t working, felt tired, and was hyper-cognizant of my finite life ahead. I wanted to take advantage of the time but I also didn’t have any energy to do so. But I got to spend a lot of time with family and friends.

I am lucky to have such a great group of friends. My roommate, Ben, was an absolute gem and barely acknowledged there was anything different going on. That is exactly how you want people to treat you when you are going through this – just hang out and joke about as per usual.
Although low energy, I had many good times having friends over, sneaking a beer, watching sports. My friends who I texted with got the dark jokes and carried on as normal. Our humour provided a sense of normalcy during a period of my life where I was quite lost. Big parts of my identity were tied up to the activities, routines and work I did previously, so it was nice to have some things remain the same.
At the end of radiation I wanted to treat myself to a trip to get this “take advantage of life” feeling out of me. I got the okay to fly to Vancouver Island, a place I had had always wanted to go and never had the time. Em and I caught a 4:30 am flight out. We got to BC and I was already feeling pretty worn out.
I pushed on and didn’t feel overly concerned.
We washed up at our hotel and set out to go meet our friend Sam for a beer. He brought us down these city steps to a cool looking brewery. But on the last step I kinda stumbled. I knew something was wrong right away.
I hadn’t stumbled because I was clumsy. I had told my foot to move but it didn’t. What followed was a massive wave of anxiety coupled with adrenaline. A few more steps and I knew I was going to have a seizure. Luckily, Sam is a paramedic and I kinda knew what to do as well.
I told him and Emily what was about to happen and then tried to guide myself down to the ground. While trying to go down I started seizing and I went out in Sam’s arms. This is called a grand mal seizure and is quite the show I’m told.
I woke up out of it and waited for the ambulance. Living life to the fullest was off to a great start. I was at the Victoria hospital for a couple of hours and luckily, they attributed it to pushing myself a little too hard and so soon after the radiation. I was put on epilepsy meds and proceeded to have an amazing but exhausting time on the island.
We were also able to stop in and meet Emily’s uncle in Nanaimo. He had been diagnosed with GBM at 30 and was alive and well over 26 years later.
I guess there is some hope out there.
Upon return I started my more extensive chemo schedule, double the dose for five days then three weeks off for six months. Em and I moved into a new place and I just took it easy. Chemo was exhausting and boring, I mostly vegged out or did little walks with family and friends. I did get terrible itching every time I was done my cycle because it turns out I was in the small percentage of people allergic to it.
(Yay, I keep winning awesome life lotteries… )
The epilepsy meds also made me very anxious and I would have near panic attacks just going to the grocery store. I was afraid of having another public seizure after Victoria. Eventually we got different meds and that took the edge off. Nothing major changed for me with Covid-19. Everyone was stuck at home but I was already a pro from having done it for chemo.
My energy levels slowly returned and presently I am fairly active during quarantine. I go in for scans every 3 months and hope for the best, and so far so good.
So what’s the point of my life now?
In the immediate aftermath, my goal of a lofty position at work with early retirement and posh vacations took a bit of hit. I still think it’s great to be ambitious but the importance of material things and societal positions dissolve quickly when faced with a shortened life expectancy.
Other things I once deemed important truly felt inconsequential for the first time. I used to say I didn’t really care about other people’s opinion that much, but I did. I always thought that it would be impossible not to, like it was an evolutionary trait humans picked up. But once confronted with the reality of death and the fact that once you’re gone, you won’t know or care, I started to embody that sentiment more.
My desire to adventure or “live life to the fullest” also changed a bit. I totally support doing that (YOLO) but I don’t have burning bucket list items I want to fit in before leaving. Maybe that will change but for me at this moment, the point is to enjoy myself and spend more time doing activities I enjoy with people I love.
Did Emily and I binge watch The Great Canadian Bake Show, effectively wasting another day of my life on reality tv? Definitely!
I guess the perspective change is that I cherish the time I have with her more than before. She was my rock during this and I can’t imagine going through it without her. From the long hours spent by my bed, the care during my treatment, the never-ending visits to the hospital – she did it all. I am so blessed to have had her by my side and am still the luckiest guy today.
This diagnosis was a reminder to slow things down and enjoy the present with her, my family and friends.
I would also like to help raise awareness and funds for brain cancer since there is still so much work to be done. It is devastating and I would not wish it upon anyone. For my one year anniversary of being cancer-free, I’d like to raise $1000 for Brain Tumour Foundation of Canada, a charity that helps people going through what I went through.
Check out my gofundme if you want to help me reach my goal, and thanks for reading!